Balance is far more than just the simple act of staying upright; it’s a complex, integrated system involving the brain, inner ear, eyes, and proprioceptors in the muscles and joints. When this delicate system falters—due to age, injury, neurological conditions, or inner ear issues—the resulting instability can dramatically impact a person’s quality of life and significantly increase the risk of dangerous falls. Fortunately, physical therapy offers a powerful, evidence-based roadmap to restoring this critical function. This isn’t a one-size-fits-all approach but a highly tailored regimen designed to retrain the body’s sensory and motor systems for greater stability and confidence in daily movement. A physical therapist, as a movement expert, assesses the root cause of the imbalance and constructs a program that systematically challenges and improves the three primary systems responsible for keeping you steady: visual, somatosensory (touch and joint position), and vestibular (inner ear).
The process begins with a detailed evaluation. This initial assessment involves testing strength, flexibility, gait pattern, and the integrity of the three balance systems. Based on these findings, the therapist develops a goal-oriented treatment plan. This plan often incorporates a blend of strengthening exercises, dynamic activities, and specialized techniques like Vestibular Rehabilitation Therapy (VRT) or targeted proprioception drills. The overall objective is not simply to manage the symptoms of unsteadiness but to fundamentally recalibrate the body’s internal sense of movement and position. This holistic approach helps patients move beyond a fear of falling and truly regain independence and enjoyment in their physical activities, whether it’s walking on uneven pavement or simply reaching for a high shelf.
Understanding the Core Components of Physical Therapy for Stability
The therapist develops a goal-oriented treatment plan.
A well-structured physical therapy program for balance improvement is built on several key components, each addressing a different aspect of the body’s ability to maintain equilibrium. The plan is always individualized, evolving as the patient progresses. Static and dynamic balance exercises form the foundation, beginning in a safe, controlled environment. Static exercises, like the single-leg stand or the tandem stance (heel-to-toe position), focus on maintaining stability in a stationary position. These foundational drills are crucial for building the core stability required for more complex movements later on. The goal is to gradually increase the hold time, moving from holding onto a sturdy surface like a countertop to being able to balance without any support for up to 30 seconds or more.
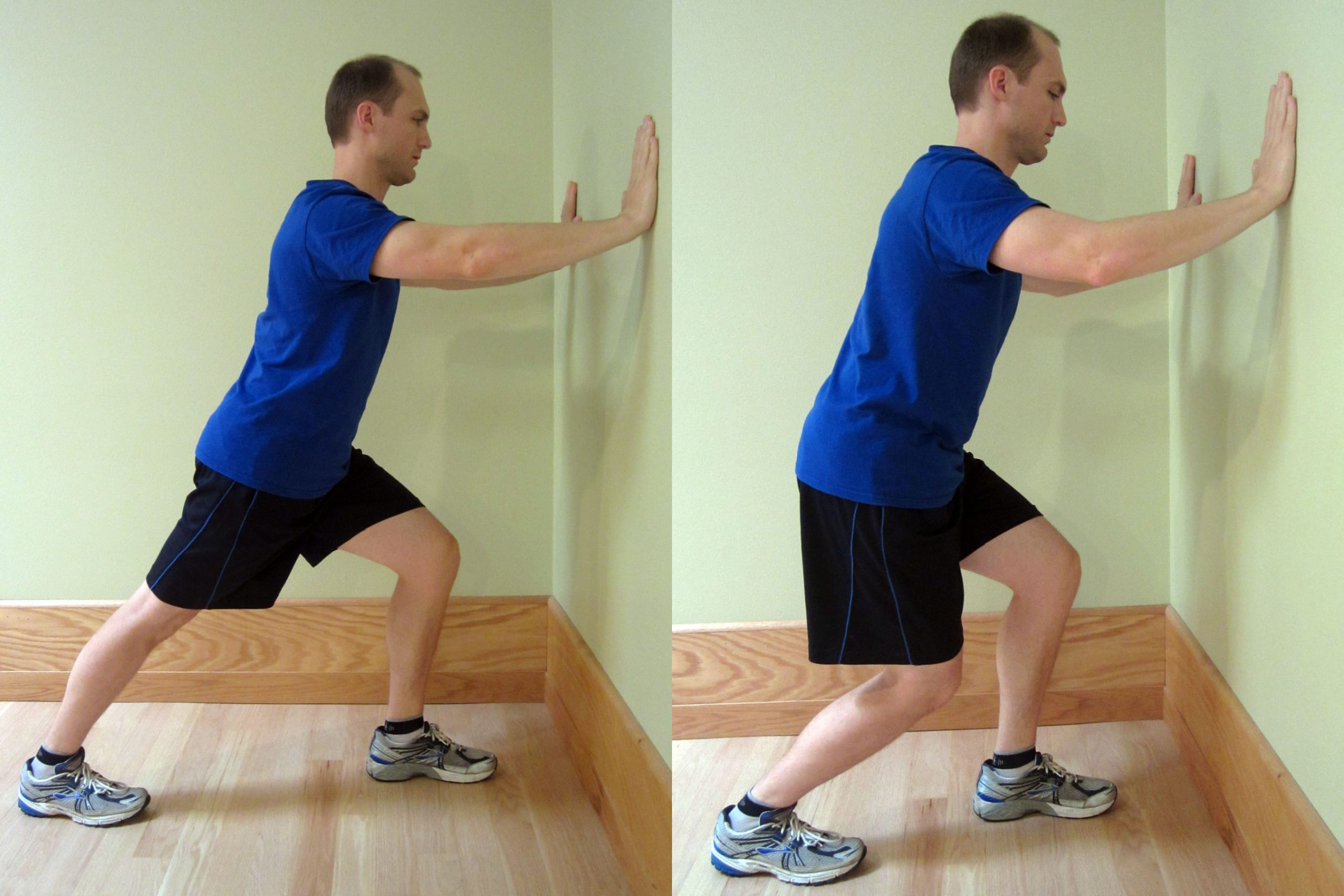
Dynamic exercises introduce movement while maintaining balance, closely mimicking real-life challenges. Activities such as weight shifts—moving weight from one foot to the other without losing form—and standing three-way kicks—lifting one leg forward, to the side, and then back—improve hip joint control and stability. Walking patterns are also refined through gait training, including the heel-to-toe walk, which forces the body to challenge its coordination and stability in a narrow base of support. These dynamic movements are essential for improving the ability to react to unexpected shifts, like stepping off a curb or quickly turning to avoid an obstacle. Strengthening exercises for the lower body and core are integrated alongside these balance drills, as weak muscles contribute significantly to instability. Exercises like sit-to-stand without using hands and various leg raises build the muscular support necessary to sustain balance and recover from a stumble.
Specializing in Sensory Retraining: Vestibular and Proprioceptive Techniques
Vestibular rehabilitation therapy is a very specific type of physical therapy to help people with balance and dizziness problems.
For individuals whose balance issues stem from inner ear problems, conditions like vertigo, labyrinthitis, or peripheral vestibular hypofunction, Vestibular Rehabilitation Therapy (VRT) becomes the central pillar of their physical therapy program. VRT is a highly specialized, exercise-based approach aimed at helping the brain compensate for damage or dysfunction in the vestibular system. This therapy operates on the principle of central compensation, encouraging the brain to rely more effectively on the visual and somatosensory systems to manage balance when the inner ear signals are unreliable. The exercises in VRT are often intentionally designed to provoke mild, controlled symptoms, a process known as habituation training, which helps the nervous system get used to and ultimately ignore movements or situations that trigger dizziness.
They often use the repetition of carefully designed visual stabilization exercises with people who have trouble reading or focusing while moving.
A critical component of VRT is gaze stabilization training, which involves moving the head while keeping the eyes fixed on a stationary target. This repetition of carefully designed visual stabilization exercises is vital for coordinating the vestibular ocular reflex (VOR), the mechanism that allows vision to remain clear even when the head is moving. By focusing on adaptation exercises, the therapist systematically challenges the VOR to improve its function. Patients may also engage in balance retraining exercises on different surfaces and with increasingly narrow bases of support, including exercises with their eyes closed to specifically enhance reliance on the often-underutilized vestibular system. This type of targeted rehabilitation is key to reducing dizziness symptoms and significantly lowering the risk of falling for those with inner ear conditions.
Proprioception training involves exercises that continually challenge the body’s awareness in space.
Beyond the inner ear and vision, the third crucial input for balance is proprioception, often described as the body’s sixth sense—the awareness of the position and movement of the body without looking at it. Proprioception training involves exercises that continually challenge the body’s awareness in space, forcing the brain to process joint and muscle input more efficiently. When this system is impaired, often following an ankle sprain or other joint injury, the brain receives poor or slow information, making quick, corrective movements difficult. Physical therapists address this by introducing activities that demand precise spatial awareness and muscle response.
Beginner proprioception exercises include single-leg balance with eyes closed, which instantly removes the visual component, forcing the somatosensory system to take over. As stability improves, the therapist might introduce unsteady surfaces using equipment like foam pads, wobble boards, or Bosu balls. Standing on a stability ball or balance board forces the smaller muscles around the ankle, knee, and hip to fire quickly and constantly make micro-adjustments to maintain equilibrium. More advanced functional exercises include cone pickups or single-leg squats, which combine balance with functional movement patterns. These exercises, tailored to the individual’s recovery needs, effectively rewire the brain-body connection, leading to a much safer and more automatic control over movement.
Integrating Functional Movement and Advanced Training
Functional balance training involves exercises that mimic daily activities.
As patients progress, the physical therapy focus naturally shifts toward functional training, which involves exercises that mimic daily activities and prepare the individual for real-world environments. This phase of rehabilitation is tailored to the specific movements and activities a person needs to return to, thereby maximizing independence. For example, practicing complex tasks like releasing and lifting objects while standing on one foot or navigating an agility ladder helps improve coordination and quick response time, skills vital for avoiding falls outside the clinic.
Tai chi is a good exercise for healthy adults to help develop balance.
The inclusion of lower-impact, mindful movement is also highly beneficial. Tai chi, a practice involving slow, deliberate, and flowing movements, is widely recognized as an excellent exercise for improving balance, reducing the fear of falling, and enhancing self-efficacy in movement, particularly in older adults. Water-based exercises in a swimming pool can also offer a safe way to build strength and improve balance due to the buoyancy that reduces the fear of impact. The physical therapist works to integrate these functional and lifestyle movements into a patient’s regular routine, ensuring that the skills learned in the clinic translate effectively to daily life.
The Role of Lifestyle and Environmental Modifications
Your physical therapist will assess problem footwear and hazards in your home.
A comprehensive balance program extends beyond exercises and must include practical advice on lifestyle and environmental modifications to reduce fall risk. Physical therapists are trained to assess a patient’s home environment, identifying and addressing potential hazards. This includes assessing problem footwear, which should be nonskid, rubber-soled, and low-heeled, and removing common tripping hazards like loose rugs, electrical cords, and poor lighting. Simple home modifications, such as adding sturdy handrails on stairs and in bathrooms, are often recommended to create a safer space.
Moreover, the therapist provides strategies for managing daily activities that typically challenge balance. This can involve teaching patients safe techniques for changing positions slowly, especially when moving from sitting to standing or after a large meal, to avoid sudden drops in blood pressure that cause dizziness. They may instruct patients on ankle-pumping exercises before standing to encourage better blood flow. These practical, non-exercise steps are just as critical as the physical drills themselves, forming a safety net that reinforces the physical gains made during therapy sessions. The goal is to move the patient toward a lifestyle that avoids too much sitting, encourages daily, challenging physical activity, and ultimately fosters a renewed sense of confidence in their body’s stability.
